Myocardial infarction (MI), commonly known as a heart attack, is a significant health concern that impacts millions of individuals worldwide. It occurs when blood flow to a part of the heart is blocked, leading to damage or death of heart tissue. Given the prevalence and severity of this condition, Myocardial Infarction ICD-10 accurate coding is essential for diagnosis, treatment, and reimbursement processes within the healthcare system.
The International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) provides a standardized coding system that helps healthcare providers document myocardial infarction effectively. This article aims to decode myocardial infarction ICD-10-CM codes, offering a comprehensive understanding of their classifications, guidelines, and clinical implications for healthcare professionals.
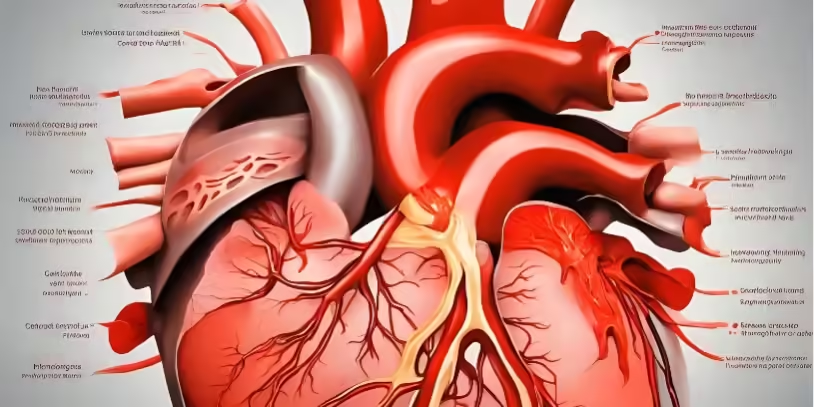
Overview of Myocardial Infarction
Definition and Pathophysiology
Myocardial infarction is defined as the irreversible damage to heart muscle due to prolonged ischemia. Ischemia occurs when blood flow to the heart is obstructed, typically by a blood clot formed at the site of a ruptured atherosclerotic plaque. This obstruction leads to a lack of oxygen and nutrients in the heart tissue, causing cell death.
The pathophysiological mechanisms underlying myocardial infarction can vary, but they commonly involve:
- Coronary Artery Disease (CAD): The most frequent cause of MI, CAD develops when the coronary arteries become narrowed or blocked over time due to plaque buildup (atherosclerosis).
- Coronary Artery Spasm: A temporary tightening of the muscles within the arteries, leading to reduced blood flow.
- Embolism: A clot or debris that travels through the bloodstream and lodges in a coronary artery, obstructing blood flow.
Types of Myocardial Infarction
Myocardial infarctions are classified into several types based on their presentation and underlying mechanisms:
- ST-Elevation Myocardial Infarction (STEMI): Characterized by significant elevation in ST-segment on an electrocardiogram (ECG), indicating a complete blockage of a coronary artery. STEMI typically requires immediate medical intervention.
- Non-ST-Elevation Myocardial Infarction (NSTEMI): Identified by less pronounced ECG changes and often indicative of partial blockage. NSTEMI may also require urgent care, but the presentation is usually less critical than STEMI.
- Myocardial Infarction Due to Coronary Artery Spasm or Embolism: These cases may involve sudden artery narrowing or occlusion due to factors unrelated to atherosclerosis.
Risk Factors
Various risk factors contribute to the likelihood of experiencing a myocardial infarction, including:
- Modifiable Risk Factors: High blood pressure, high cholesterol levels, smoking, diabetes, obesity, physical inactivity, and unhealthy diet.
- Non-modifiable Risk Factors: Age, gender, and family history of cardiovascular disease.
Understanding these risk factors is crucial for both prevention strategies and clinical management of patients at risk for myocardial infarction.
Introduction to ICD-10-CM Coding
What is ICD-10-CM?
The International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) is a coding system used by healthcare providers to document diagnoses, including myocardial infarction. It provides a standardized way to classify and code medical conditions, facilitating accurate communication among healthcare providers, insurers, and researchers.
The structure of ICD-10-CM codes consists of an alphanumeric format, where the first character is a letter, followed by two digits and, in many cases, additional characters for specificity (e.g., I21.9).
Importance of Accurate Coding
Accurate coding is critical in the healthcare landscape for several reasons:
- Clinical Documentation: Proper coding ensures that patient records accurately reflect their medical history and treatment, which is essential for ongoing patient care.
- Reimbursement: Payers rely on accurate coding to determine reimbursement levels for services provided, impacting the financial health of healthcare facilities.
- Public Health Reporting: Accurate coding contributes to population health statistics and helps monitor trends in diseases, including myocardial infarction.
Classification of Myocardial Infarction ICD-10-CM Codes
Overview of Myocardial Infarction Codes
The specific codes related to myocardial infarction are found primarily in the I21 category of ICD-10-CM. These codes provide a standardized way to document various types of myocardial infarctions and are essential for effective treatment and management.
Breakdown of Myocardial Infarction Codes
The ICD-10-CM codes for myocardial infarction include:
- I21.0 – ST elevation myocardial infarction of anterior wall
- I21.1 – ST elevation myocardial infarction of inferior wall
- I21.9 – Acute myocardial infarction, unspecified
Each of these codes has specific criteria based on the type, location, and presentation of the myocardial infarction, which healthcare providers must understand to code accurately.
Additional Codes Related to Myocardial Infarction
In addition to the primary myocardial infarction codes, there are related codes that may be utilized:
- I22 – Subsequent myocardial infarction: This code is used for instances where a patient experiences a new MI following a previous one.
- I25 – Chronic ischemic heart disease: This code may apply when documenting underlying chronic conditions that contribute to acute myocardial infarction.
Coding Guidelines for Myocardial Infarction
General Coding Guidelines
When selecting the appropriate ICD-10-CM code for myocardial infarction, healthcare providers should adhere to the following guidelines:
- Specificity: Choose the most specific code available based on the type of myocardial infarction and its characteristics.
- Timeline: Determine whether the myocardial infarction is acute, subacute, or old. The timeline significantly influences the code selection.
Use of Additional Codes
When coding myocardial infarction, additional codes may be necessary to capture related complications or conditions. For example:
- If the patient experiences heart failure following a myocardial infarction, the relevant heart failure code should be included alongside the MI code.
Clinical Documentation Requirements
Thorough documentation is crucial for accurate coding. Healthcare providers should ensure that clinical records clearly outline:
- The type of myocardial infarction (STEMI or NSTEMI).
- Any related conditions or complications.
- The patient’s medical history, including risk factors and previous cardiovascular events.
Clinical Implications of Myocardial Infarction Coding
Impact on Patient Care
Accurate coding directly impacts patient care and management. It helps healthcare providers:
- Determine the appropriate treatment plan.
- Monitor patient outcomes and effectiveness of interventions.
- Facilitate communication among interdisciplinary teams involved in patient care.
Reimbursement and Billing
The way myocardial infarction is coded affects reimbursement from both Medicare and private insurers. Accurate coding ensures:
- Timely reimbursement for services rendered.
- Minimization of claim denials and appeals.
Quality Reporting and Metrics
Myocardial infarction codes play a significant role in quality reporting initiatives. Proper coding contributes to:
- Benchmarking against quality measures.
- Identification of areas for improvement in patient care and outcomes.
Best Practices for Myocardial Infarction Coding
Education and Training
Ongoing education and training are vital for healthcare professionals to stay updated on ICD-10-CM coding practices. Regular workshops and seminars can enhance understanding and coding accuracy.
Multidisciplinary Collaboration
Collaboration among healthcare providers, coders, and billing specialists is essential for optimizing coding practices. Effective communication ensures:
- Accurate documentation of patient encounters.
- Timely and appropriate coding of diagnoses and procedures.
Regular Audits and Compliance Checks
Conducting regular audits of coding practices can help healthcare organizations identify trends and areas for improvement. Feedback from audits should be utilized to refine processes and enhance accuracy.
Future Trends in Myocardial Infarction Coding
Advances in Coding Systems
As healthcare continues to evolve, coding systems may also undergo changes. Staying informed about potential modifications to ICD-10-CM coding guidelines is essential for healthcare providers.
Importance of Continued Education
The landscape of healthcare coding is constantly changing. Healthcare professionals should prioritize continuous education to ensure compliance with the latest guidelines and practices.
Frequently Asked Questions
What is the primary ICD-10-CM code for myocardial infarction?
The primary ICD-10-CM codes for myocardial infarction are found under the I21 category, with specific codes like I21.0 for ST elevation myocardial infarction of the anterior wall and I21.9 for acute myocardial infarction, unspecified.
How do I determine the appropriate code for a myocardial infarction?
To determine the appropriate code, healthcare providers must assess the type of myocardial infarction (e.g., STEMI vs. NSTEMI), its location, and any associated complications or prior events.
What is the difference between STEMI and NSTEMI coding?
STEMI (ST-Elevation Myocardial Infarction) is coded differently than NSTEMI (Non-ST-Elevation Myocardial Infarction) due to the distinct clinical presentations and treatment implications. For example, STEMI may be coded as I21.0, while NSTEMI is typically coded as I21.4.
What documentation is required for accurate coding of myocardial infarction?
Accurate documentation should include the type of myocardial infarction, relevant clinical findings, treatment administered, and any complications or associated conditions.
Are there additional codes needed when coding myocardial infarction?
Yes, additional codes may be required for complications, such as heart failure (I50.0–I50.9) or chronic ischemic heart disease (I25.0–I25.9), depending on the patient’s clinical scenario.
What are the coding guidelines for myocardial infarction?
Guidelines include selecting the most specific code available, considering the timeline of the myocardial infarction (acute, subacute, or old), and ensuring thorough documentation to support the coding choices.
How does accurate coding of myocardial infarction impact patient care?
Accurate coding ensures appropriate treatment plans, influences care pathways, and affects the monitoring of patient outcomes, ultimately enhancing the quality of care delivered.
What are the consequences of incorrect coding for myocardial infarction?
Incorrect coding can lead to claim denials, reimbursement issues, potential audits, and negatively impact patient care due to misrepresentation of clinical conditions.
How can healthcare professionals stay updated on changes in coding guidelines?
Healthcare professionals can stay updated by participating in training programs, attending coding workshops, subscribing to relevant healthcare publications, and utilizing online resources and coding updates from CMS (Centers for Medicare & Medicaid Services).
What resources are available for learning more about myocardial infarction coding?
Resources include the American Academy of Professional Coders (AAPC), the American Health Information Management Association (AHIMA), coding textbooks, official ICD-10-CM guidelines, and online training courses focused on coding practices.
Final Thoughts
Decoding myocardial infarction ICD-10-CM codes is essential for healthcare providers involved in diagnosing and managing patients with this critical condition. Accurate coding not only ensures proper reimbursement but also enhances the quality of care provided to patients. By prioritizing education, collaboration, and continuous improvement, healthcare professionals can optimize their coding practices, ultimately leading to better patient outcomes.
Key Market Player
Ready to optimize your medical billing and boost your revenue? Look no further. Zmed Solutions LLC is your trusted partner in professional Medical Billing Services.
Join hundreds of satisfied healthcare providers who have already elevated their revenue with our expert services. Don't miss out on what could be your practice's most profitable decision.
Schedule a Consultation Today!
Contact Us Now, and experience the difference. Your financial success starts here!